Understanding Multiple Sclerosis (MS)
Multiple sclerosis (MS) is a disease of the brain and spinal cord. Right now, there is no cure for MS. But there are many treatments to help manage it. Many people with MS can manage their symptoms and lead active, healthy lives. Read on to learn more about MS and its treatments.
What is MS?
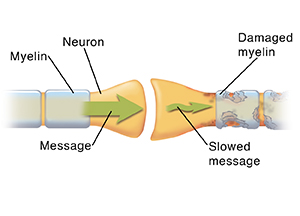
The brain is the body’s control center. Each part of the brain controls specific functions. These include movement, balance, sensation, and thinking. The brain controls these by sending and receiving messages through nerves. Nerves have a protective covering. The covering is called myelin. With MS, the myelin on nerves in the brain and spinal cord is damaged. The loss of this covering causes messages moving along affected nerves to slow or stop. This results in MS symptoms.
Causes and risk factors for MS
Experts don't know what causes MS. But most research suggests that the body’s immune system attacks and destroys myelin by mistake. MS most often begins in adults between ages 20 and 40. It happens in women more often than men. It is more likely to occur in a person with a family history of MS. Many genes have been found that raise the risk of MS. A past infection with Epstein-Barr (mononucleosis) is more common among people with MS. Those who smoke, have vitamin D deficiency, or childhood obesity are more likely to develop MS.
Types of MS
There are four main types of MS. These are:
-
Relapsing-remitting MS. This type of MS is the most common. It causes episodes of symptoms (also called attacks or flare-ups). Periods of part or full recovery follow these attacks. Each attack may be worse than the one before it.
-
Primary-progressive MS. This type of MS has a slow onset of symptoms that get worse over time. Generally, there are no periods of recovery or only temporary minor improvements.
-
Secondary-progressive MS. This type of MS starts as relapsing-remitting MS. After a stable period, the disease gets worse. About 50% of people with relapsing-remitting MS have secondary-progressive MS within 10 years of their first attack. About all of them have it within 25 years.
-
Progressive-relapsing MS. This type of MS includes symptoms that slowly get worse, and periods of flare-ups together.
Symptoms of MS
MS symptoms vary from person to person. The types of symptoms depend on which nerves are affected. They also depend on how much nerve damage there is in the brain and spinal cord. A person can have different symptoms during the course of the disease. Symptoms can include:
-
Extreme tiredness (fatigue)
-
Numbness, tingling, or loss of feeling
-
Pain
-
Muscle spasms or weakness in the arms, legs, or both
-
Vision problems, such as rapid eye movements, double vision, or vision loss
-
Balance and coordination problems
-
Problems walking or moving the arms, legs, or both
-
Bowel and bladder control problems
-
Problems with sexual function
-
Dizziness
-
Trouble concentrating, focusing, or remembering things
-
Trouble reasoning and solving problems
-
Trouble speaking or swallowing
-
Depression
Diagnosing MS
Tests to diagnose MS include:
-
MRI. This test shows detailed pictures of the brain and spinal cord. It helps check for areas of damaged nerves. These are called lesions or plaques.
-
Evoked potential tests. A type of evoked potential test, called visual evoked potentials, may be done to show how well your optic nerves are working.
-
Spinal tap. This is also called lumbar puncture. It checks the fluid around your brain and spinal cord for signs of nerve sheath damage (demyelination).
-
Blood tests. These help rule out other causes of the symptoms.
Treating MS
The goal of treatment is to manage your symptoms and slow the rate at which the disease worsens. You can manage your symptoms in these ways:
-
Medicines. Some medicines help keep your body’s immune system from attacking the myelin. This may reduce how often attacks happen. And it may reduce how bad they are. Other medicines help control symptoms or ease pain when attacks happen.
-
Rehabilitation (rehab). Symptoms from MS can affect daily living. Rehab includes physical, occupational, and speech therapy. These can help you maintain strength and function. If needed, your healthcare provider will prescribe a cane, walker, or wheelchair. You can make changes in your work or living space to improve your safety.
-
Supportive services. Counseling and support groups help you cope with the challenges of living with MS. Family members and friends may also benefit from these services.
-
Lifestyle changes. Making some changes in your lifestyle and daily routine may help you manage symptoms. This includes getting enough rest and regular exercise. It includes eating healthy foods and reducing stress. It's helpful to figure out things that trigger MS episodes and avoid them.
-
Other treatments. Researchers are exploring new treatments for MS. Many of these are in clinical trials. This means they are being tested for safety and to see how well they work. Talk with your providers about treatments that might be an option for you.
Long-term concerns
MS is an unpredictable disease. Each person's experience is different. In general, you should have regular visits with your provider. They will watch your symptoms. They will review how well your medicines and other treatments work. MS symptoms may get worse as your disease progresses. If this happens, you may need more care and treatments.
Online Medical Reviewer:
Heather M Trevino BSN RNC
Online Medical Reviewer:
L Renee Watson MSN RN
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Date Last Reviewed:
7/1/2024
© 2000-2026 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.