Understanding Systemic Lupus Erythematosus (Lupus)
Systemic lupus erythematosus is an autoimmune disease that causes your body’s immune system to attack its own cells and tissues. It can affect your joints and nervous system. It can affect blood vessels. And it can affect organs, such as the skin, kidneys, lungs, and brain. It can cause rashes, extreme tiredness (fatigue), pain, and fever. Severe lupus can harm organs and cause other serious problems, including death.
Lupus is an ongoing (chronic) disease. It can be mild to severe. It is most common in young adult women. But it can occur in people of any age.
Lupus has no known cure. But medicines may help manage symptoms. You can also help manage lupus by living a healthy lifestyle and working with your healthcare provider.
What causes lupus?
The immune system makes proteins called antibodies. These protect the body against bacteria, viruses, foreign bodies, and cancer cells. In some people, the immune system makes antibodies that attack the body’s own cells and tissues. This leads to inflammation and tissue damage in the body. This is what happens in lupus as well as some other autoimmune diseases.
The cause of lupus is unknown. But genetics and other factors, such as certain viruses and allergies, may play a role.
Symptoms
Lupus can appear in many parts of the body. Because of this, it can affect people in different ways. You may have only some of these symptoms. You are not likely to have all of them. Some of the common symptoms of lupus are:
-
Fatigue
-
Fever
-
Sores in the mouth or nose
-
Patchy hair loss
-
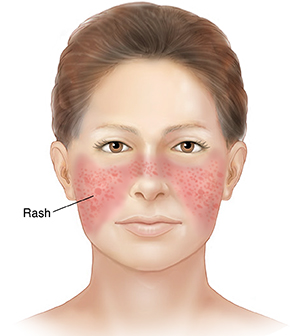
Butterfly-shaped rash on the cheeks of the face (malar rash)
-
Rashes caused by sunlight
-
Swollen or painful joints (arthritis)
-
Muscle pain
-
Weight loss
-
Heartburn (acid reflux)
-
Stomach pain
-
Less blood flow in the fingers and toes
-
Headaches
-
Feeling dizzy
-
Abnormal amounts of blood cells
-
Bruising or bleeding
-
Depression
-
Confusion
Severe symptoms can include:
-
Swelling in legs and ankles (edema)
-
Inflammation of tissue around the lungs that causes chest pain when breathing (pleurisy)
-
Inflammation of the lining of the heart (pericarditis)
-
Seizures
-
Kidney problems
-
Miscarriage
-
Abnormal amounts of blood cells
What is remission?
Remission is when symptoms go away for a period of time. Lupus can go into remission. If lupus flares up again, your symptoms may return the same as before.
Possible complications of lupus
Lupus can cause harm to the body over time. This can lead to serious problems, such as:
-
Kidney disease (lupus nephritis). Over time, this can lead to kidney failure. Kidney failure is treated with dialysis or kidney transplant. Kidney disease can cause certain symptoms. Call your healthcare provider if you have swelling in your hands, feet, or around your eyes. Also tell your healthcare provider if you have changes in urination. These include needing to go more often, pain when you urinate, excessive bubbles in the urine, or dark urine.
-
Clogged arteries (atherosclerosis). This raises a person’s risk for heart attack, heart failure, and stroke. To help lower your risk for these problems, you can make certain lifestyle changes. Stop smoking, if needed. Also get your blood pressure, diabetes, and cholesterol under control. Stay active and healthy.
Diagnosing lupus
Lupus may be challenging to diagnose. This is because it has many possible symptoms that could have other causes. And the symptoms can happen slowly over time.
To diagnose lupus, your healthcare provider will do a physical exam. They will also ask about your health history, your family's health history, and your symptoms. You will have tests to help confirm the diagnosis. The tests may include:
-
Antibody blood tests. These tests are done to look for certain kinds of antibodies in your blood. The main test for lupus is the antinuclear antibodies (ANA) test. Most people (97%) with lupus will have a positive ANA test result. If the ANA test is positive, other antibody tests may also be done.
-
CBC blood test. This test measures the amount of red blood cells, white blood cells, and platelets. These levels may all be low. This is common in lupus.
-
Other blood tests. These may be done to look for other problems, such as how certain organs are working. Some look for signs of inflammation in the body. Some tests look for certain kinds of proteins. Other tests check how fast your blood clots.
-
Urine tests. These are to look for blood or protein in the urine. This can mean your kidneys are not working normally.
-
Biopsies. A biopsy is when small samples of tissue are taken from the affected area and checked under a microscope. To look for signs of lupus, biopsies may be done of the skin and kidneys. The test looks for a group of proteins called autoantibodies found in the blood of people with lupus. This test alone does not diagnose lupus. But it can help confirm a diagnosis.
Treating lupus
Lupus is treated in many ways. You may work with a rheumatologist. This is a healthcare provider who specializes in lupus, arthritis, and other related autoimmune diseases. You may also work with other kinds of healthcare providers. These include primary healthcare providers and specialists in kidney disease, blood disorders, immune disorders, and heart problems. You may also meet with a social worker to help you manage your treatment plan. The goals of treatment include treating symptoms, preventing flare-ups of lupus, and helping reduce damage to the body.
Your healthcare provider may give you medicine to help treat symptoms. Medicines are not a cure. But they can help prevent organ damage or suppress the disease. Your healthcare provider will prescribe one or more medicines to help you feel better. Be sure to take them as directed. You may be given medicines, such as:
-
Nonsteroidal anti-inflammatory drugs (NSAIDs). These can be used to help relieve swelling, pain, and fever.
-
Antimalarial medicine. A medicine used to prevent and treat malaria can help ease some lupus symptoms. It can treat fatigue, rashes, joint pain, and mouth sores. The medicine may also help prevent blood clots.
-
Corticosteroid (steroids) medicines. These medicines lower inflammation and can help people when lupus affects the kidneys, lungs, heart, or nervous system.
-
Medicines that suppress the immune system. These can help treat severe symptoms of lupus that have attacked organs.
-
Other medicines. A medicine called a biologic may be a choice. Clinical trials are also being done to test other medicines that may help people with lupus.
Talk with your healthcare providers about the risks, benefits, and possible side effects of all medicines.
Managing your health
Lupus can also be managed by keeping a healthy lifestyle. Here are ways to take care of yourself:
-
Find the right balance of rest and activity.
-
Eat plenty of vegetables, fruits, and grains.
-
Stay at a healthy weight.
-
Exercise a few times a week, at least. Try walking, swimming, or biking.
-
Learn ways to reduce or manage stress.
-
Stay out of the sun as much as you can. Use sunscreen with SPF 15 or higher.
-
Quit smoking if you currently smoke.
-
Stay educated and current on lupus information.
Work with your healthcare provider to manage your lupus. Be sure to see your provider for regular checkups and tests.
Pregnancy and lupus
If you are a person of child-bearing age, talk with your healthcare provider about the risks of pregnancy and lupus. It is advised that your disease is under control or in remission for 6 months before you become pregnant. Pregnancy is considered very risky for people with lupus who have any of these:
Lupus symptoms can flare up during pregnancy. Since pregnancy with lupus is high risk, you will need extra care from your healthcare team. You will need to see a high-risk pregnancy specialist. This is an OB-GYN (obstetrician-gynecologist) who has additional training in managing high-risk pregnancies. You may need to see your provider more often.
Getting support
Lupus is a chronic disease. It can put special demands on your life. Family and friends can be a good source of help and support. You may also want to join a support group for people with lupus. By talking with other people who have lupus, you may learn new ways to cope. You may also feel less alone. For more information, contact the following: