A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
Hysterosalpingogram (HSG)
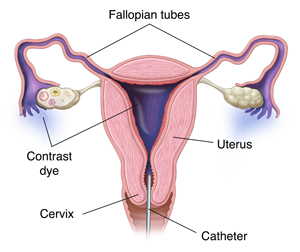
HSG (hysterosalpingogram) is an X-ray test used to view your uterus and fallopian tubes. It’s most often used to help diagnose why you are not able to get pregnant. HSG is done in the X-ray center of a hospital or clinic. During the procedure, your gynecologist or a radiologist (a doctor who specializes in the use of X-rays) takes images as a contrast dye flows through the uterus and fallopian tubes. The dye makes it easier to see these organs on X-rays. It can also help pinpoint the location of problems. In some cases, your healthcare provider will be present during the test. HSG usually takes less than 30 minutes. You can often go back to your normal routine within a short time.
How to say it
HIHS-tuh-roh-sal-PIHNG-oh-gram
Why might I need HSG?
HSG is used to diagnose problems with the fallopian tubes and uterus. These can include:
-
Blockage or narrowing of the fallopian tubes
-
Scarring of the fallopian tubes and uterus
-
Abnormalities in the shape and size of the fallopian tubes and uterus
-
Growths in the uterus
What are the risks?
Problems with HSG are rare but can include:
How do I get ready for HSG?
The procedure will be scheduled shortly after the end of your menstrual period. This helps ensure you are not pregnant. When you schedule your test, tell your healthcare provider if you have allergies to iodine, contrast materials, foods, medicines, dyes, or preservatives. Tell your provider about any past surgeries and recent illnesses. Also tell them what medicines you are taking. You will be asked to sign a consent form and may want to arrange for a ride home after the procedure. In some cases, you’ll be given antibiotics to take before and after the test. A day or 2 before the exam, your healthcare provider may ask you to:
This procedure should not be done if you have an active inflammatory condition. Tell your doctor or technologist if you have a chronic pelvic or vaginal infection or an untreated sexually transmitted infection at the time of the procedure.
What happens during HSG?
-
You will be asked to lie on an X-ray table with your knees bent—much like a Pap test.
-
An instrument called a speculum is inserted into the vagina to hold it open.
-
The cervix may be numbed. Then a catheter (thin tube) is guided through the cervix and into the uterus. In some cases, the cervix may need to be dilated first to widen the cervical opening.
-
The X-ray machine will be positioned over your abdomen. Then, contrast dye is injected through the catheter.
-
The dye may stretch the uterus and tubes, causing some cramping or pain.
-
As the dye flows through the uterus and tubes, X-rays are taken and displayed on a monitor. You may be able to watch the progress of the dye on the monitor. You might be asked to change positions.
-
It is normal for some dye to spill out of the tubes and be absorbed by the body. The rest may appear later as vaginal discharge.
What happens after HSG?
-
If you feel lightheaded or dizzy, you can rest on the table until you’re ready to get dressed.
-
You will likely have a thick discharge as some of the dye drains out of the uterus. You may have a small amount of bleeding for a day or two. Use pads, not tampons, until the discharge is gone.
-
For a few hours you may feel some cramping. This can usually be relieved with over-the-counter pain medicines.
-
You may be told not to have sex or douche for a day or two.
After the radiologist has studied the X-rays, your healthcare provider will talk with you about the results of your HSG. This may be later the same day or during a follow-up appointment. In some cases, more tests may be needed to look more closely at your reproductive organs. Your healthcare provider may also recommend medicine or surgery to help correct a problem.
When should I call my healthcare provider?
Contact your healthcare provider if you have any of the following:
-
Severe pelvic pain or pelvic pain that gets worse
-
Heavy vaginal bleeding. This means more than a pad an hour for 2 hours.
-
Vomiting
-
Fever of 100.4°F (38°C) or higher, or as advised by your provider
-
Foul-smelling or unusual vaginal discharge
Date Last Reviewed:
8/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.