DVT Prevention: Intermittent Pneumatic Compression (IPC)
Deep vein thrombosis (DVT) is a clot in the deep veins of your leg. It can cause swelling, pain, and tenderness in your leg. A piece of the blood clot can break off and travel to your lungs. This may cause a serious and life-threatening condition called a pulmonary embolism.
What is intermittent pneumatic compression?
Intermittent pneumatic compression (IPC) uses a simple machine to help prevent DVT. The device has two sleeves that automatically fill with air and painlessly squeeze your legs. This increases blood flow through the veins of your legs and helps prevent blood clots.
Why IPC is used
In most cases, IPC is done in the hospital. You may need IPC to lower your risk for DVT if you have:
-
Had a recent surgery.
-
A health condition that limits your ability to move, such as an injury or a stroke.
-
An injury to a deep vein in one of your legs.
-
An inherited blood disorder that increases blood clotting.
IPC is one way to help prevent DVT. A blood-thinning medicine, such as warfarin, may also be prescribed to help lower your risk for DVT. This medicine may work better than the compression device in preventing DVT, but it may increase the risk of bleeding. IPC and blood thinners are often used together.
Risks of IPC
The risks of IPC include:
Skin care can help prevent these complications. People with certain health conditions should not use IPC devices. For example, people with leg ulcers, burns, or some conditions affecting the arteries and veins of the legs (peripheral vascular disease) have a higher risk for problems. Older adults may be more at risk for skin sores. Talk with your doctor about which risks apply most to you.
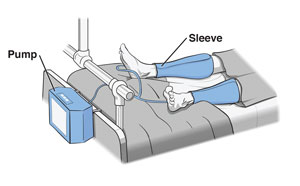
What happens during IPC
There are many types of IPC devices. The sleeves may cover your calves, or they may go around your thighs and calves. A nurse or aide will apply the IPC sleeves. They may show you how to take the sleeves off and put them back on. When fastened around your legs, the sleeves should feel snug, but they shouldn’t be too tight. You should be able to place a finger between the sleeves and your legs.
Next the sleeves are attached to the compression machine. The machine will cycle between inflating and deflating the sleeves. This may feel a little strange at first. Let your nurse or aide know if it's uncomfortable.
Call for help if you need to get up to use the bathroom, go for a walk, or take a shower. Your nurse or aide will help you take off your sleeves before you leave your bed and put them back on when you return to your bed. If your doctor or nurse has told you not to get up on your own, don't leave your bed without help from staff. Always take off the sleeves completely before leaving your bed.
Tell your doctor or nurse right away if:
-
You have swelling, pain, or redness in either of your legs.
-
You have a sore on the skin under either of the sleeves.
-
The sleeves feel too tight or cause pain.
After IPC
Your doctor will tell you when you can stop using the IPC device. This will be when you have less of a risk for DVT.
Your doctor may give you other directions about ways to help prevent DVT. These may include being as active as possible and moving your legs, ankles, and feet when you are inactive. Follow all of your doctor’s instructions.