Bronchiolitis
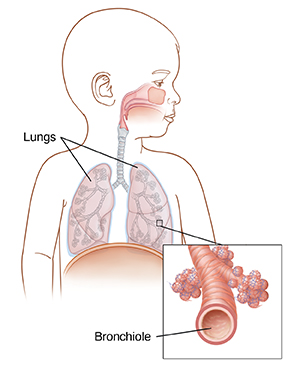
Bronchiolitis is an inflammation in the lungs. It affects the small breathing tubes (bronchioles). It's most common in children under 2 years of age. Children tend to get better after a few days. But in some cases, it can lead to severe illness. So a child with this lung infection must be treated and watched carefully. Bronchiolitis is not the same as bronchitis. Bronchitis is an infection of the larger, central airways.
What is bronchiolitis?
Bronchiolitis is an infection that involves the small breathing tubes of the lungs. The most common cause is respiratory syncytial virus (RSV), but it can be caused by other viruses. The virus causes the very small bronchioles to become inflamed, swollen, and filled with fluid. In small children, this can lead to trouble breathing and feeding. The symptoms start out like those of a common cold. They include stuffy and runny nose, sneezing, and a mild cough. Over a few days, your child may develop wheezing, trouble breathing, and a fever.
How is bronchiolitis treated?
Antibiotics are not used to treat bronchiolitis unless a bacterial infection is present. Your child's healthcare provider may prescribe saline nose drops to help clear the mucus. In severe cases, your child may need to stay in the hospital. Your child may get IV (intravenous) fluids, oxygen, and breathing treatments.
How can I prevent the spread of bronchiolitis?
The viruses that cause bronchiolitis spread easily. They can be spread through touching, coughing, or sneezing. To help stop the spread of infection:
-
Wash your hands with warm water and soap often. Or use alcohol-based hand cleaners. Do this before and after touching your child, before and after preparing food, and before and after treating a cut. Also wash your hands after changing diapers, coughing or sneezing, using the toilet, touching garbage, or touching or feeding a pet.
-
Scrub hands for at least 20 seconds with clean, running water and soap. If you need a timer, sing the Happy Birthday song through twice. Make sure to wash the backs of your hands, between your fingers, and under your fingernails. Dry your hands well.
-
Teach other family members and caregivers about proper handwashing. Have people wash their hands before touching your baby.
-
Keep your child away from other children while they're sick.
-
Don't share cups or utensils with anyone who's sick.
When to call the healthcare provider
Call healthcare provider right away if your child:
-
Has symptoms that get worse
-
Has a deep, harsh-sounding cough
-
Refuses to drink fluids or seems dehydrated (such as no urination in 8 hours, no tears when crying, "sunken" eyes, or dry mouth)
-
Appears overly tired when trying to breathe
-
Has a fever (see "Fever and children" below)
Call 911
Call 911 right away if your child is:
-
Breathing faster than normal, or has wheezing or a whistling sound with breathing
-
Difficult to wake up
-
Unable to speak or swallow
-
Having trouble breathing
-
Has blue, purple, or gray skin or lips
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years old, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4°F (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older