A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of conditions beginning with that letter.
Click 'Topic Index' to return to the index for the current topic.
Click 'Library Index' to return to the listing of all topics.
Bacterial Infection of the Nose and Sinuses
A bacterial infection of the nose and sinuses is sometimes called acute bacterial rhinosinusitis. Acute means that you’ve had symptoms for less than 4 weeks. But you may have them for up to 12 weeks.
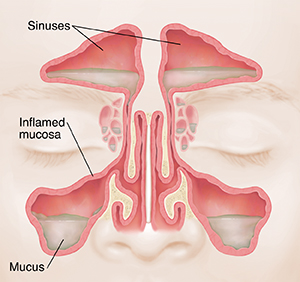
Understanding your sinuses
The nasal cavity is the large air-filled space behind your nose. The sinuses are a group of spaces formed by the bones of your face. They connect with your nasal cavity. A bacterial infection can cause the tissue lining these spaces to become inflamed. Mucus may not drain normally. This leads to face pain and other symptoms.
What causes a bacterial infection of the nose and sinuses?
This type of infection most often occurs after an upper respiratory infection, such as a cold. Bacteria then infect the lining of your nasal cavity and sinuses. But you can also get it if you have:
Symptoms of a bacterial infection of the nose and sinuses
The symptoms may be different for each person. They may include:
-
Nasal congestion or blockage.
-
Pain or pressure in the face.
-
Thick, colored drainage from the nose.
Other symptoms you may have are:
Diagnosing a bacterial infection of the nose and sinuses
Your health care provider may diagnose you with this type of infection if you’ve had an upper respiratory infection like a cold for 10 or more days with symptoms that don't get better, or get worse. Your provider will ask about your symptoms and your past health. They will check your vital signs, such as your temperature. You’ll also have an exam. The provider will check your ears, nose, and throat. You likely won’t need any tests. If the infection comes back, you may have other tests.
Treatment for a bacterial infection of the nose and sinuses
Treatment may include:
-
Antibiotics. This medicine treats the bacterial infection. If your provider prescribed antibiotics, take them as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
-
Nasal corticosteroid medicine, for short-term use. Drops or spray used in the nose can reduce swelling and congestion. This treatment is most likely to help people with underlying allergies.
-
Over-the-counter pain medicine. This is to ease sinus pain and pressure. Talk with your provider before taking any over-the-counter medicines.
-
Nasal decongestant medicine. Spray or drops may help to ease congestion. Don't use them for more than a few days.
-
Salt wash (saline irrigation). This can help to loosen mucus.
Possible complications of a bacterial infection of the nose and sinuses
This bacterial infection may come back or become long-term (chronic). In rare cases, it may cause problems, such as:
-
Inflamed tissue around the brain and spinal cord (meningitis).
-
Inflamed tissue around the eyes (orbital cellulitis).
-
Inflamed bones around the sinuses (osteitis).
These problems may need to be treated in a hospital. You may need intravenous (I.V.) antibiotic medicine or surgery.
When to contact your doctor
Contact your provider right away if:
-
You have a headache.
-
You have a fever of 100.4°F (38°C) or higher, or as directed by your provider.
-
You have a stiff neck.
-
You have trouble seeing.
-
You have swelling around your eyes.
-
You have confusion or trouble staying awake.
-
Your symptoms don’t get better, or get worse.
-
Your symptoms don’t get better after 3 to 5 days on antibiotics.
Online Medical Reviewer:
Daphne Pierce-Smith RN MSN
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Sravani Chintapalli Researcher
Date Last Reviewed:
4/1/2025
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.