A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
Preventing Deep Vein Thrombosis After Surgery
In the days and weeks after surgery, you have a higher chance of developing a deep vein thrombosis (DVT). This is a condition in which a blood clot (thrombus) forms in a deep vein. They are most common in the leg. But a DVT may form in an arm or another deep vein in the body. A piece of the clot, called an embolus, can separate from the thrombus and travel to the lungs. A blood clot in the lungs is called a pulmonary embolus (PE). This can cut off the flow of blood to part or all of the lungs. It's a medical emergency and may cause death.
Doctors use the term venous thromboembolism (VTE) to describe both DVT and PE. They use the term VTE because the two conditions are very closely related and their prevention and treatment are similar.
Prevention in the hospital or other facility
Your doctor will usually prescribe one or more of the following to prevent blood clots:
-
Blood-thinner (anticoagulant). This medicine prevents blood clots. You take it by mouth, by injection, or through an I.V. (intravenous). Commonly used anticoagulants include warfarin and heparin. Newer anticoagulants may also be used, including rivaroxaban, apixaban, dabigatran, and enoxaparin. Sometimes the doctor may not give you an anticoagulant medicine. It's important that they discuss the risks and benefits with you.
-
Compression stockings. These elastic stockings fit tightly around your legs. They help keep blood flowing toward your heart by the pressure they apply. They prevent blood from pooling and forming blood clots. When you first put them on, the stockings may be uncomfortable. But after a while, you should get used to them.
-
Exercises. Simple exercises while you are resting in bed or sitting in a chair can help prevent blood clots. Move your feet in a circle or up and down. Do this 10 times an hour to improve circulation.
-
Getting out of bed and walking (ambulation). After surgery, a nurse will help you out of bed as soon as you are able. Moving around improves circulation and helps prevent blood clots.
-
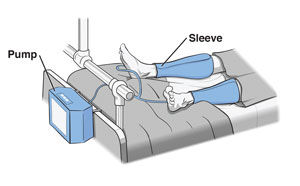
Sequential compression device (SCD) or intermittent pneumatic compression (IPC). Plastic sleeves are wrapped around your legs and connected to a pump that inflates and deflates the sleeves. This applies gentle pressure to promote blood flow in the legs and prevent blood clots. These should be worn when you lie in bed or sit in a chair.
Prevention at home
 |
| Ankle exercises can help keep blood flowing in the veins. |
Deep vein thrombosis can happen even after you go home. Follow all instructions from your doctor. The following are some general guidelines about DVT prevention:
-
Blood-thinner medicine. If a blood thinner was prescribed, make sure you follow all directions about taking it. Be sure you know what foods and medicines may interact. And ask your doctor what to do if you forget to take a dose.
-
Compression stockings. Your doctor will tell you how often to wear and remove the stockings. Follow all instructions closely. Each time you remove your stockings, check your legs and feet for red areas or sores. If you see any changes, call your doctor right away.
-
Returning to activity. Follow all instructions about returning to activities. Be as active as you can. This improves blood flow and helps prevent a clot from forming. When in bed or in a chair, continue with the ankle exercises you did in the hospital.
-
Sequential compression device (SCD) or intermittent pneumatic compression (IPC). In some cases, this device may be recommended at home. If you are using this device at home, make sure you closely follow all instructions from your doctor. You will be instructed on how often and for how long to use the device. Remove the sleeves if you are up and walking.
When to call your doctor
You may have symptoms of a blood clot. Or you may have signs of bleeding from medicines to prevent clots.
Contact your doctor right away if you have:
-
Pain, swelling, or redness in the leg, arm, or other area.
-
Blood in your urine or stool.
-
Very dark or tar-like stool.
-
Vomiting with blood.
-
Bleeding from the nose.
-
Bleeding from the gums.
-
A cut that won't stop bleeding.
-
Bleeding from the vagina.
Call 911
Call 911 if you have:
Online Medical Reviewer:
Esther Adler
Online Medical Reviewer:
Mahammad Juber MD
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Date Last Reviewed:
6/1/2025
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.