Pericarditis
What is pericarditis?
The pericardium is the sac-like covering around the heart. It helps protect the heart from infection and allows the heart to move smoothly during each heartbeat. It consists of two thin layers of tissue with a small amount of fluid, called the pericardial fluid, between them. When these layers become inflamed, they can rub against the heart. This causes chest pain. Pericarditis most often happens after a respiratory infection. It occurs in people of all ages but is more common in men ages 20 to 50 years.
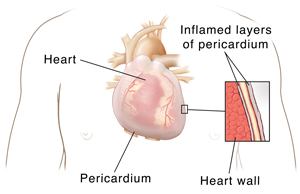 |
| With pericarditis, the inflamed layers of the pericardium rub against the heart. This results in pain and other symptoms. |
What are the symptoms of pericarditis?
Pericarditis can be short-term (acute) or long-term (chronic). The acute type occurs suddenly and typically lasts days or up to 3 weeks. The chronic type develops over time and lasts for more than 3 months. Symptoms can vary between the types.
What causes pericarditis?
In many cases, the cause is unknown (idiopathic pericarditis). Possible causes include:
-
Viral infection. This is a common cause, often after a viral respiratory infection.
-
Bacterial or fungal infection.
-
Autoimmune diseases, such as scleroderma and lupus.
-
Recovery from a heart attack.
-
Injury or surgery to the chest, esophagus, or heart.
-
Radiation treatment to the chest.
-
Certain types of cancer.
-
HIV/AIDS.
-
Medicines that suppress the immune system.
-
Kidney failure.
How is pericarditis diagnosed?
The health care provider will review your health history and ask you to describe your symptoms. You’ll also have a physical exam. Your provider will listen to your heart to see if it makes certain sounds called pericardial rub. You may have these tests:
-
Electrocardiogram (ECG). This test records the electrical activity of your heart. During an ECG, small sticky pads (electrodes) are placed on your chest, arms, and legs. Wires connect the pads to a machine that records your heart's electrical signals. Pericarditis has a specific pattern that can be seen on an ECG. But it often needs more testing to confirm.
-
Lab tests. Samples of blood or pericardial fluid may be taken and tested in a lab. These tests can help find the cause of pericarditis.
-
Imaging tests of the heart or chest. These may include X-ray, MRI, and CT scans. They create pictures of the heart or the inside of the chest. An MRI scan uses magnets and radio waves. A CT scan uses detailed X-ray images and a computer.
-
Echocardiogram (echo). This test creates a moving picture of the heart using ultrasound technology. During an echo, a probe moved over the chest sends out harmless sound waves. These create a picture that shows the size and shape of the heart. It shows how well the heart is working. It also shows if fluid has built up in the tissue around the heart.
How is pericarditis treated?
Treatment depends on how severe the condition is and what caused it. Treatment can address the symptoms or the cause of pericarditis. It can also address the complications the condition may cause.
-
Treatment of symptoms. For minor symptoms, rest may be the only treatment needed. To relieve pain and inflammation, medicine may be prescribed. These include aspirin and ibuprofen. If pain is severe, a strong anti-inflammatory called colchicine may be prescribed.
-
Treatment of the cause, if known. For instance, antibiotics may be prescribed if the cause is a bacterial infection.
-
Treatment of complications. Serious but uncommon complications can result from both acute and chronic pericarditis. These include:
-
Cardiac tamponade. Fluid builds up within the layers of the pericardium. This can keep the heart from working as it should. And it prevents the right amount of blood flow to the body. To treat this condition, a needle is inserted into the chest wall and between the layers of the pericardium to remove the extra fluid. Sometimes surgery may be done to remove some of the pericardium.
-
Constrictive pericarditis. Over time, scar-like tissue forms in the pericardium. The tissue prevents the heart from expanding enough when it beats. This keeps the heart from working as it should. Surgery to cut or remove the pericardium is often the only treatment.
When should I seek medical care?
Get medical care right away if you have any symptoms of pericarditis. This is especially important if you have chest pain or trouble breathing. Without treatment, this condition can be life-threatening.
Online Medical Reviewer:
Rita Sather RN
Online Medical Reviewer:
Shaziya Allarakha MD
Online Medical Reviewer:
Stacey Wojcik MBA BSN RN
Date Last Reviewed:
3/1/2025
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.