A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of conditions beginning with that letter.
Click 'Topic Index' to return to the index for the current topic.
Click 'Library Index' to return to the listing of all topics.
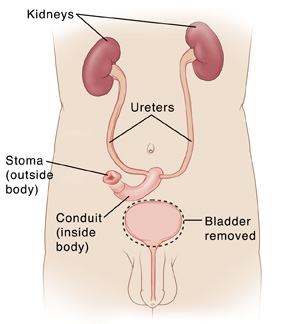
Total Cystectomy with Incontinent Urinary Diversion in Men
Total cystectomy is surgery to remove the bladder. It's most often done to treat bladder cancer. After the bladder is removed, the surgeon must make a new way to drain urine from your body. This is called urinary diversion. With incontinent urinary diversion, urine drains through a hole in your abdomen into a bag. Continent urinary diversion involves creating an internal storage for urine. It's discussed in a different information sheet.
Changes to your body
Total cystectomy and urinary diversion result in permanent changes to your body:
-
During a simple cystectomy, the bladder is removed. During a radical cystectomy, nearby lymph nodes and organs that the cancer may spread to are also removed. These may include some reproductive organs, such as the prostate and seminal vesicles. Removal of these organs can lead to problems with sexual function, including the ability to get or keep an erection. It can also cause infertility. Your healthcare provider can tell you more about this and your options.
-
After the surgery, urine no longer leaves the body through your urethra. Your ureters will be linked to a piece of intestine that is brought out of the belly. This is called a stoma and is where the urine can drain out of the body. Urine then passes through the stoma and drains into a bag worn outside the body, under your clothes. You’ll need to wear a bag all of the time. And you’ll need to empty and change the bag regularly. You’ll also need to take care of your stoma and the skin around it. You’ll be taught how to do this while you’re in the hospital.
-
This surgery causes physical changes, but it may also bring up difficult feelings. People report a variety of emotional reactions to a cancer surgery. These range from feelings of being overwhelmed to denial, anger, sorrow, anxiety, hope, and gratitude. How you were raised may determine your response. You may feel the need to be strong, turn to others for support, rely on professionals, or turn to your faith. There is no right emotion or best way to cope. It’s important to do what is right for you and not compare yourself to others. If you are struggling with the prospects of this surgery, ask your care team for help.
Preparing for surgery
Get ready for the surgery as you have been told. In addition:
-
Tell your health care provider about all prescription and over-the-counter medicines, vitamins, herbs, and supplements you take. This includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may need to stop taking some or all of them before surgery, as directed by your provider.
-
Don't eat or drink during the 8 hours before your surgery. This includes coffee, water, gum, and mints. (If you have been instructed to take medicines, take them with a small sip of water.)
-
If you have been told to, prepare your bowel for surgery (“bowel prep”). This process starts 1 to 2 days before the surgery. Your healthcare provider may tell you to restrict your diet to clear liquids. You may also be asked to take laxatives or to give yourself an enema. Follow all instructions you are given.
The day of surgery
The surgery takes 4 to 6 hours. Afterward, you will stay in the hospital for 5 to 7 nights.
Before the surgery starts
-
An IV (intravenous) line is put into a vein in your arm or hand. This delivers fluids and medicine such as antibiotics. In some cases, a central or arterial line is inserted into a vein somewhere else on the body. Your health care provider can tell you more.
-
You may get medicine to prevent blood clots in your veins.
-
To keep you free of pain during the surgery, you’re given general anesthesia. This medicine allows you to comfortably sleep through the surgery. A tube may be inserted into your throat to help you breathe.
-
You may have an epidural to help control post-surgery pain. A small tube is inserted into your back to deliver pain medicine that numbs the lower body. Talk to your doctor, anesthesiologist, or nurse anesthetist about this option.
During the surgery
-
An incision is made in the lower abdomen.
-
The lymph nodes near the bladder are removed. These are checked for cancer cells (a sign that cancer has spread).
-
During a simple cystectomy, the bladder is removed. During radical cystectomy, certain nearby organs, such as the prostate, are also removed. If possible, nerves that affect sexual function are spared.
-
A piece of your large or small intestine is removed. This is used to make a conduit for the urine to flow from the ureters out of the body. If a piece of small intestine is used, this is called an ileal conduit. If a piece of large intestine is used, this is called a colon conduit. With either type, one end is connected to the ureters. The other end is brought through an incision in the abdominal wall to form the stoma.
-
When the surgery is complete, the incisions are closed with stitches or staples.
-
A small tube (drain) may be placed near the incisions. This drains fluid that may build up after the surgery.
-
Tubes called stents may be placed through the stoma into the ureters. These help drain urine until healing is complete.
Recovering in the hospital
After the surgery, you will be taken to the postanesthesia care unit (PACU) to be closely monitored as you awake from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. When you are awake and stable, you will be taken to your hospital room. While in the hospital:
-
You will be given medicine to manage pain and any nausea. Let your providers know if your pain or nausea is not controlled.
-
You’ll first get IV fluids. In a day or so, you will start on a liquid diet. You will then slowly return to a normal diet.
-
As soon as you’re able, you will get up and walk. This reduces the risk of potential problems such as blood clots in the legs.
-
You’ll be taught coughing and breathing techniques to help keep your lungs clear and prevent pneumonia.
-
An ostomy nurse will show you how to care for your stoma and bag. Make certain the person who will be caring for you at home after the surgery attends this education. Ask for printed material with pictures showing how to care for the stoma and bag.
-
Drains and stents will likely be removed while you are in the hospital. If not, you will be shown how to care for them at home.
-
Make sure to get a contact number for the healthcare provider, ostomy nurse, and hospital before going home. This is in case you have problems or questions after the surgery.
Recovering at home
You will be sent home with an adult family member or friend. Have someone stay with you for the next few days. Recovery time varies for each person. Your health care provider will tell you when you can return to your normal routine. Until then, follow the instructions you have been given. Be sure to:
-
Take all medicines as directed.
-
Care for your incision and stoma as instructed.
-
Follow your health care provider’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that cause the incision to be covered with water until your provider says it’s okay.
-
Don't lift anything heavy or do strenuous activities, as directed.
-
Don't drive until your provider says it’s okay. Don't drive if you’re taking medicines that make you drowsy or sleepy, including pain medicines.
-
Walk a few times daily. As you feel able, slowly increase your pace and distance.
-
Don't strain to pass stool. If needed, take stool softeners as directed by your provider.
-
Drink plenty of water every day. This helps prevent urine odor and dehydration.
Many times, patients feel overwhelmed and have trouble remembering everything they were taught about daily life with the stoma. If you feel this way, a special source of patient support, called an ostomy visitor, may be helpful. This is a person who has had a surgery similar to yours and has adapted to the changes it caused. They can answer many questions about day-to-day life after surgery. If this type of person would be helpful to you, ask your care team how to get such support.
When to contact your health care provider
Contact your health care provider or seek medical care right away if:
-
You have chest pain or trouble breathing. ( Call 911).
-
You have a fever of 100.4° F ( 38°C ) or higher, or as directed by your provider.
-
You have unusual pain, redness, swelling, bleeding, or drainage at the incision site.
-
You have pain, redness, swelling, odor, or drainage at the stoma site.
-
You have decreased or no urine output for longer than 4 hours.
-
You have bloody urine with clots.
-
You have pain that can't be controlled with medicines.
-
You have nausea or vomiting that doesn’t go away.
-
You have pain or swelling in the legs.
-
You have new symptoms that concern you or your caretaker.
-
You have emotional distress such as depression, anxiety, anger, or fear.
Follow-up care
You will have follow-up visits so your health care provider can check how well you’re healing. Stitches, staples, or tubes will be removed. You and your provider can also discuss any further treatment you may need. If you are having trouble adjusting to your stoma and bag, talk to your provider or ostomy nurse. You may also want to consider a support group for people with stomas. Ask your provider for more information.
Risks and possible complications
-
Bleeding (may require a blood transfusion)
-
Infection
-
Blood clots
-
Pneumonia or other lung problems
-
Failure to remove all of the cancer, or cancer comes back
-
Problems with the stoma
-
Abnormal levels of vitamins or minerals in the blood, requiring lifelong medicine
-
Scarring and narrowing of the ureters
-
Bowel obstruction
-
Problems with sexual function or with fertility
-
Risks of anesthesia (your anesthesiologist will discuss these with you)
Online Medical Reviewer:
Lalitha Kadali Researcher
Online Medical Reviewer:
Melinda Murray Ratini DO
Online Medical Reviewer:
Rita Sather RN
Date Last Reviewed:
12/1/2024
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.