Brachial Plexus Injuries
What is a brachial plexus injury?
The brachial plexus is a bundle of connected nerves in the neck region coming from your spine. It branches under the clavicle (collarbone) down into your chest, shoulders, arms, and hands. This group of nerves controls the motions of your shoulder, wrists, hands, and arms. The nerves let you do things like raise your arm, type on your keyboard, and throw a baseball.
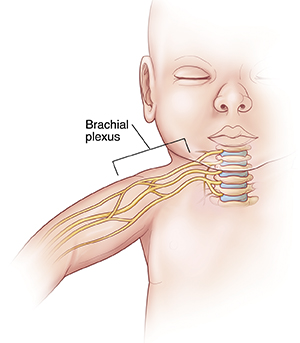
The brachial plexus nerves are sensory, too. For example, they let you know that a pan you grab with your hand is too hot to hold.
The brachial plexus can be injured in many different ways from pressure, stress, or being stretched too far. The nerves may also be damaged by cancer or radiation treatment. Brachial plexus injuries can happen to babies during childbirth. In some cases, an overactive immune system can damage the plexus.
Brachial plexus injuries cut off all or part of the communication between the spinal cord and the arm, wrist, and hand. This may mean that you can't move or feel parts of your arm or hand. Often, brachial plexus injuries cause pain or a total loss of feeling in the area.
The severity of a brachial plexus injury varies. In some people, function and feeling returns to normal. Others may have lifelong disability because they can't use or feel a part of the arm.
Brachial plexus injuries are categorized as type:
-
Avulsion. The root of the nerve is completely separated from the spinal cord (the most severe type).
-
Neurapraxia. The nerves are stretched (the least severe type).
-
Rupture. Part of the nerve is actually torn.
-
Neuroma. Scar tissue forms on the stretched nerve as it fixes itself.
-
Brachial neuritis. This is a rare syndrome for which no cause can be identified. It's also called Parsonage-Turner syndrome.
Brachial plexus birth injury happens when the brachial plexus gets stretched during childbirth. It is called Erb palsy or Klumpke palsy, depending on which part of the plexus is injured. Erb palsy affects 1 or 2 babies in every 1,000 births.
What causes a brachial plexus injury?
The most common cause of this injury is when the neck is tilted while pulling (traction) happens on the other side of the neck. But the causes of injury vary, including motor vehicle accidents, falls, gunshot wounds, athletic injuries (especially contact sports), and childbirth.
During childbirth, large babies may be at an increased risk for brachial plexus injuries. A quick or emergency delivery, when the baby must be forcibly pulled out, can cause a brachial plexus injury. This happens because the baby's neck is often flexed severely in one direction. Babies in breech position (bottom end comes out first) and those whose labor lasts an unusually long time may also suffer brachial plexus injuries.
Cancer and radiation therapy can cause brachial plexus injury. The tumor itself can invade the brachial plexus. Radiation of lymph nodes in the area can also damage the nerves.
Autoimmune disorders can sometimes cause the immune system to attack the plexus.
Who is at risk for a brachial plexus injury?
Factors that may raise your risk are:
-
Motor vehicle accidents.
-
Sports activities, especially football.
-
Childbirth, especially large babies, breech position, or long labor.
-
Cancer and radiation therapy.
What are the symptoms of a brachial plexus injury?
Symptoms depend on where along the length of the brachial plexus the injuries happen and how severe they are.
Common symptoms of brachial plexus injuries are:
-
No feeling in the hand or arm.
-
Pain in the arm or hand.
-
Inability to control or move the arm, wrist, or hand.
-
An arm that hangs limply.
How is a brachial plexus injury diagnosed?
A doctor will examine your hand and arm. They will test for feeling and function to help diagnose this type of injury.
Other diagnostic tests include:
-
Imaging tests, such as an ultrasound (sonogram), MRI, or CT scan.
-
Tests to determine nerve function and electrical activity, including a nerve conduction study and electromyogram.
-
X-ray of the neck and shoulder area.
How is a brachial plexus injury treated?
Some brachial plexus injuries need surgery to repair the damage. Physical therapy can help you restore function in your arms and hands. It can also improve range of motion and flexibility in stiff muscles and joints.
Brachial plexus injuries don't always need treatment. Some people, especially babies with a brachial plexus birth injury, get better without any treatment. But it can take as long as several months for the injury to heal. Certain exercises can help with healing and function.
You may need regular checkups to watch the progress and healing of a brachial plexus injury. Checkups are especially important for babies. They may be needed for as long as 2 years as the injury heals.
In some cases, a surgeon can connect other nerves or tendons to the muscles of the arm or hand to restore function. This is only done when the chance of spontaneous nerve growth becomes unlikely.
Medicine may be used if your doctor thinks you may have an autoimmune condition.
What are possible complications of a brachial plexus injury?
Brachial plexus injuries often heal well if they aren't severe. Many people with minor brachial plexus injuries recover between 90% and 100% of the normal function of their arms.
For severe brachial plexus injuries, surgery may be needed right away to try to get function back. Without it, you might have a lasting disability and be unable to use your arm or hand.
If you have a brachial plexus injury that causes a lack of feeling, you must take special care when dealing with hot items, razors, knives, or other objects that could harm you. A brachial plexus injury can keep you from feeling any other injury to the affected area. You may not notice that you're hurt.
You may also have long-term pain or sensory changes in the affected area. Or you could have paralysis.
What can you do to prevent a brachial plexus injury?
To help prevent these injuries:
When to contact your doctor
If you have had an injury to the neck or shoulder area and you can't feel or move your hand or arm, contact your doctor to find out what's causing your symptoms. Get assessed and diagnosed right away to help prevent permanent damage.
Key points about brachial plexus injury
-
The brachial plexus is a bundle of connected nerves in the neck region coming from your spine. This group of nerves controls the motions of your shoulder, wrists, hands, and arms.
-
Brachial plexus injuries cut off all or part of the communication between the spinal cord and the arm, wrist, and hand. This may mean that you can't move or feel parts of your arm or hand.
-
The most common cause of this injury is when the neck is tilted while pulling (traction) happens on the other side of the neck. But the causes of injury are varied.
-
Some brachial plexus injuries need surgery to repair the damage. Physical therapy can help you restore function in your arms and hands.
-
Get assessed and diagnosed right away to help prevent permanent damage.
Next steps
Tips to help you get the most from a visit to your doctor:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your doctor tells you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your doctor gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your doctor if you have questions, especially after office hours or on weekends and holidays.